Etiology
Malaria is caused by protozoae of the genus Plasmodium. It was
traditionally believed that there are only four species that cause human malaria:
Plasmodium falciparum, P. malariae, P.ovale and P.vivax. (WHO, 2013). A fifith
species was isolated in 2010 and has been named P. knowlesi. (Kantele
A, 2010). The four species have distinct morphological differences that aid in
their diagnosis on a blood smear. (CDC, 2013).
Malaria is vector borne and the parasites can be
transmitted by more than thirty species of Anopheline mosquitoes.
Epidemiology
Malaria is endemic in 104 countries . (WHO, 2012)
The average incubation period for malaria is 12
days (tropical strains) and 15 days (Temperate strains). (Lover AA,
2013)
Malaria
is severe in children , immunosuppressed patients and pregnant women. Malaria
in pregnant women can cause miscarriages, stillbirths and neonatal death. (WHO,
2013)
Lifecycle
Infectious sporozoites of the Plasmodium are
carried by the Anopheles mosquito in its salivary glands. When the mosquito
feeds on a human, it injects saliva and the sporozoites into the body. The
sporozoites moves to their predilection site , the liver. There the sporozoites
enter the hepatocytes and divide. They produce thousands of merozoites , which
are haploid forms. These rupture the hepatocytes as they exit and enter the
blood stream.
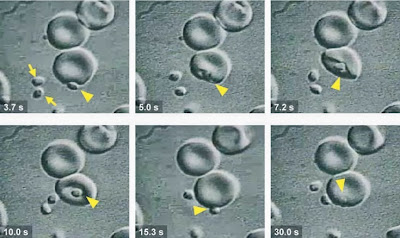
Erythrocyte invasion by merozites (Haldar et al.,2007)
The intraerythrocytic cycle of Plasmodium is clinically important. The receptors on the erythrocytes include Thrombospondin, CD36, ICAM-1, VCAM-1 and ELAM-1.(Pasloske, 1994). The erythrocytes infected with mature stages of Plamodium adhere to vascular endothelial cells in postcapillary venules. Infected erythrocytes can also form rosettes with uninfected erythrocytes. In P.falciparum, the paraite matures to a trophozoite stage, which matures into schizonts, which eventually relaease 16-32 daughter merozoites on rupturing the RBC. These merozoites invade uninfected erythrocytes and the cycle continues.
Malaria : Clinical stages
The acute disease presents as a febrile sickness.
(WHO,2013). The intra erythrocytic cycle of the parasite is reflected as a
cyclic pattern of fevers and chills. Other features of the disease include
hypoglycemia, hyperlactermia, anemia and altered consciousness (Weatherall DJ, 2002 ; Haldar, 2006). Levels of TNF alpha are high in malaria patients.
TNF alpha enhances the expression of ICAM-1, VCAM-1 and ELAM-1 and is
responsible for causing prodromal symptoms such as fever and nausea (Pasloske, 1994)
The most severe disease is caused by P. falciparum.
Clinical signs are nonspecific and include fever, chills, headaches, myalgia,
vomoitng, cough , abdominal pain. Complications that arise from this infection
include acute renal failure, pulomnary oedema, convulsons, shock, coma and
death. Cerebral malaria is a complicated form of
Plasmodium falciparum infection, found especially in children.
Malaria
caused by P.vivax and P.ovale are not as life threatening as falciparum malaria but are the major cause for relapsing
malaria. These protozoae can remain dormant in the liver as persistent liver
forms called hypnozoites. (WHO,2013)
Diagnosis
The
WHO recommends definitive diagnosis either on the basis of microscopy or rapid
diagnostic tests.Plasmodium species can be detected on blood smears stained by simple Romanowsky stains such as Giemsa. Blood smears are easy and inexpensive to make. This method allows detection of various stages of the parasite and a rough quantification of parasite density. (WHO, 2013)
The Rapid Detection Tests detect specific antigens in the serum/blood. These tests can detect a single species at a time or multiple Plasmodium species.
Treatment
The disease is entirely preventatble and treatable. According to the " Guidelines for the Treatment of Malaria " Handbook published by the WHO in 2010, Arteminisin based combination therapies are recommended for uncomplicated cases. Combination therapies include Artemininsin in combination with lumefantrine, amodiaquine, mefloquine, sulfadoxine-pyrimethamine. Duration of therapy must be atleast seven days.
Second line treatments recommended are artesunate with tetracycline/ doxycycline / clindamycin for 7 days.
Prevention
The
main method of prevention so far has been vector control. Mosquitoes can be
eliminated by insecticide spraying on breeding grounds. Transmission can be
prevented by the use of individual insecticide treated mosquito nets.
Vaccines
Subunit vaccines against
malaria are being evaluated in clinical trials. These will be explored in subsequent posts.
malaria]. Duodecim. 2010;126(4):427-34.
Weatherall DJ, Miller LH, Baruch DI, Marsh K, Doumbo OK, et al. 2002.
Malaria and the red cell. Hematology
Am. Soc. Hematol. Educ. Program 1:35–57
Pasloske BL, Howard RJ. Malaria, the red cell and the endothelium. Annu Rev Med. 1994; 45: 283-95
Haldar K, Murphy SC, Milner DA, Taylor TE. Malaria : mechanisms of erythrocytic infection and pathological correlates of severe disease. Annu Rev Pathol. 2007; 2 : 217-49
Lover AA, Coker RJ. Quantifying effect of geographic location on
epidemiology of Plasmodium vivax malaria.
Emerg Infect Dis [Internet]. 2013 JulPasloske BL, Howard RJ. Malaria, the red cell and the endothelium. Annu Rev Med. 1994; 45: 283-95
Haldar K, Murphy SC, Milner DA, Taylor TE. Malaria : mechanisms of erythrocytic infection and pathological correlates of severe disease. Annu Rev Pathol. 2007; 2 : 217-49
WHO World Malaria Report 2012 (who.int/malaria/publications/world_malaria_report_2012/en/)
No comments:
Post a Comment