I started my research for this post under the assumption that I was soon going to be buried under a ton of clinical articles and good-practice reviews about Cryptosporidium infections in dogs. I came away bitterly disappointed at the utter lack of clinical pointers.I had fully expected a well defined, pathognomonic diagnostic finding , to have been developed and published under the aegis of one Veterinary Association or the other. Unfortunately, that does not seem to be the case.
Ordinarily, when a case presents with diarrhea, a vet would try to narrow down the possible causes, . A list called the "Differential Diagnosis List" is (mentally) made which is conveniently divided into infectious and non infectious etiological agents that could have caused the clinical sign(s). Agents are eliminated based on clinical evidence and the results of the tests at the clinician's disposal. 'Cryptosporidiosis' is listed among the glorified ranks of Tritrichomonas foetus, Giardia sps, Balantidium coli and metazoans under the broad category of 'Parasites that cause diarrhea' in that definitive guide of lists, called "Differential Diagnosis in Small Animal Medicine"(edited by Gough A.). Listing the disease and not the agent is still a thing of great curiosity to me. On the list that runs six pages, Cryptosporidium has scored a spot. If Cryptosporidium caused diarrhea in dogs frequently, it would earn a firm place on the DD list of every veterinarian.
However, allow me make a statement that seems to defy all clinical logic, but is firmly within the grasp of commonly understood parasitology knowledge : Cryptosporidium canis, C. parvum and C. meleagridis (all of which have been found in dogs) do not always seem to produce "clinical" disease in dogs. They are typical parasites, carried along for the journey, which do not really harm the host. They seem to favour featuring in multiple etiology dramas, playing the roles of supporting parasites, neither sufficient nor necessary, over the role of protogonist parasites that direct the ebb and flow of the disease.
To treat this "disease" in dogs with the commonly available coccidiostats would be utterly silly and would cast a clinician in poor light , because the parasite is technically not a Coccidian to begin with. The taxonomy tempests have not been stilled on the displacement of Cryptosporidium from the Coccidian Apicomplexans.
Now, for a brief review of clinical research.
In 2000, the "Dog genotype" was validated by phylogenetic analysis of 18S and HSP70 as the new species, Cryptosporidium canis . (Morgan et al., 2000). Publications have implicated C.canis as the causal agent in both canine and human patients, including a case of a HIV infected human patient who harboured the canine genotype. (Pieniazek et al., 1999) But, how clinically relevant these are, is highly debatable
In the first infection report of Cryptosporidiosis in a week old pup, published in 1983, the authors include this disclaimer, "Cryptosporidia may have played a role in the enteritis seen in this pup, but further studies are needed to establish its pathogenecity". That is, the fact that they saw organisms that resembled Cryptosporidium could have been a happy coincidence, or in strict Pathology terms, "an incidental finding" that masked an insidious underlying cause. (Wilson et al., 1983) It has been established since that "Morphology is not a reliable tool for delineating species within Cryptosporidium" (Fall et al., 2003). Thus, it is impossible to know, which species of Cryptosporidium had infected the pup or if there had been another agent , say CPV that had coinfected it.
In a paper published in the Journal of American Animal Hospital Association in 1999, Willard and Bouley describe the fatal case of an immunocompromised 8 wk old dog that was coinfected with Cryptosporidium and other Coccidia. Which came first - the immunocompromise or the infection - is unknown.
Titilincu et al., in a paper titled "Prevalence of Cryptosporidium Spp. in asymptomatic dogs by ELISA and risk factors associated with infection" , published in Lucrari Stiiniifice Medicina Veterinara Vol XLIII (I) , in 2010 maintain that 53% of the 374 sampled dogs were positive on the ELISA, but were clinically asymptomatic. The positive animals when serotyped, were found to be infected with C.canis.
In a longitudinal study (from birth to 1 year of age) published in Acta Veterinaria Scandinavica in 2007 by Hamnes et al., Cryptosproridium was found by immunofluorescent staining in 44.1% of the 290 sampled animals from Norway. Since they used a direct FITC conjugated MAb against C.parvum, the samples identified were of course exclusively C.parvum. Again, the glaringly obvious point in the study is the complete lack of clinical data to support a clinical infection.
Despite the above mentioned studies, the jury is still out on the importance of Cryptosporidium sps. as a pathogenic agent in dog diarrhea, and we are left to ponder on these questions that will still haunt us:
1. Does Cryptosporidium canis actually cause disease in dogs?
2. What percentage of the cases harbour other enteric pathogens?
3. Do detection methods matter? Is it better to perform a PCR on a clinical sample than to perform a ZN staining on it ?
4. Should all cases that are positive using PCR be prescribed coccidiostats irrespective of clinical status ?
5. Should we add the agent to our DD list just to be safe ?
While some answers are obvious, others require a fair bit of clinical and lab research. To assume that answers will be obtained without both working together is obviously foolish.
References :
Morgan UM, Xiao L, Monis P, et al. Cryptosporidium spp. in domestic dogs: the "dog" genotype. Appl Environ Microbiol 2000;66:2220-2223.
Pieniazek NJ, Bornay-Llinares FJ, Slemenda SB, et al. New cryptosporidium genotypes in HIV-infected persons. Emerg Infect Dis 1999;5:444-449.
Fall A, Thompson RC, Hobbs RP, et al. Morphology is not a reliable tool for delineating species within Cryptosporidium. J Parasitol 2003;89:399-402.
Wilson RB, Holscher MA, Lyle SJ. Cryptosporidiosis in a pup. J Am Vet Med Assoc1983;183:1005-1006.
Thursday, December 26, 2013
Friday, December 13, 2013
A change of direction
The end of the semester is in sight. I had maintained this blog for the MICR756 class and had focused my attention on the 'Public Health Aspects of a complex Apicomplexan disease', viz. Malaria. Over the course of the semester, I found that I liked maintaining a blog and that I actually liked this sort of unofficial scientific writing.
So, from January, the blog will move to a new URL : apicomplexity.blogspot.com and will include topics starring other less known (and according to me, more interesting) apicomplexans such as Cryptosporidium, Isospora etc.
Thank you, all, for your patience. A special thanks to Dr.Nathan Fisher for the idea of a blog .
Thank you, all, for your patience. A special thanks to Dr.Nathan Fisher for the idea of a blog .
Tuesday, November 19, 2013
One Health - Policy
A determinant by another name is a problem that must be overcome
Many of the determinants involved in the spread of malaria can be controlled by policy. For example, in areas of Africa where malaria transmission is unstable (seasonal transmission, low intensity, low immunity among the population, affecting all ages), irrigation patterns affect transmission by affecting (increasing) the number of vectors available at a particular location. Mosquitoes breed well in the water logged soil of rice fields, increasing malaria transmission, although the very purpose of irrigation is to increase food productivity. (Ijumba, 2001) The authors have elegantly called this the 'paddy paradox'. Issues like this are at the very core of the dilemma of achieving all the goals of the One Health Initiative. Because all life is linked in an intricate network, a policy that affects one area inevitably affects another, in a veritable 'circle of life'.
Collaborative efforts and critical areas
One of the Manhattan principles on 'One World, One Health' really caught my eye. It states that "Forming collaborative relationships among governments, local people, and the private and public (i.e. non-profit) sectors" will "meet the challenges of global health and biodiversity conservation." (CDC,2004). To discuss the need for collaboration is great, but the only thing that will sustain the collaboration is (mandatory) policy that will hold collaborators to their promises.
In a manner similar to the one adopted for HPAI (UNDG,2008)., a coordinated global response policy for malaria must focus on critical areas that include :
a. Preventing a epidemic by controlling malaria transmission and preparing for future epidemics by improving malaria surveillance.
b. Rapidly detecting the disease, treating it and preventing its sustained spread from the index case to others
References :
1. Adamson S, Marich A, Roth I. One Health in NSW: coordination of human and animal health sector management of zoonoses of public health significance. N S W Public Health Bull 2011;22:105-112.
2. Ijumba JN, Lindsay SW. Impact of irrigation on malaria in Africa: paddies paradox. Med Vet Entomol 2001;15:1-11.
3. "Bill & Melinda Gates Foundation." Malaria. Gates Foundation, Seattle, 2013. Web. 18 Nov. 2013.
4. "MCH Programs Overview." MCH Programs Overview. Washington, 2013. Web. 19 Nov. 2013.
5. "The Manhattan Principles." cdc.gov. CDC, Atlanta, 2004. Web. 19 Nov. 2013.
6. "Contributing to One World, One Health.*" Undg.org. United Nation Development Group, 2008. Web. 19 Nov. 2013.
Many of the determinants involved in the spread of malaria can be controlled by policy. For example, in areas of Africa where malaria transmission is unstable (seasonal transmission, low intensity, low immunity among the population, affecting all ages), irrigation patterns affect transmission by affecting (increasing) the number of vectors available at a particular location. Mosquitoes breed well in the water logged soil of rice fields, increasing malaria transmission, although the very purpose of irrigation is to increase food productivity. (Ijumba, 2001) The authors have elegantly called this the 'paddy paradox'. Issues like this are at the very core of the dilemma of achieving all the goals of the One Health Initiative. Because all life is linked in an intricate network, a policy that affects one area inevitably affects another, in a veritable 'circle of life'.
Collaborative efforts and critical areas
One of the Manhattan principles on 'One World, One Health' really caught my eye. It states that "Forming collaborative relationships among governments, local people, and the private and public (i.e. non-profit) sectors" will "meet the challenges of global health and biodiversity conservation." (CDC,2004). To discuss the need for collaboration is great, but the only thing that will sustain the collaboration is (mandatory) policy that will hold collaborators to their promises.
In a manner similar to the one adopted for HPAI (UNDG,2008)., a coordinated global response policy for malaria must focus on critical areas that include :
a. Preventing a epidemic by controlling malaria transmission and preparing for future epidemics by improving malaria surveillance.
b. Rapidly detecting the disease, treating it and preventing its sustained spread from the index case to others
c. Ensuring that all essential services are continually available in the event of an outbreak
Whose responsibility is it anyway?
Policies must be put in place for the things discussed above. But, who is responsible for drafting such policies? Will these policies form a basis for laws that could be legislated by different governments? Will the local government that holds executive powers enforce such laws created by a Legislature? Will such laws/policies be upheld by local branches of the Judiciary? Or will the policies only be convention among the involved parties?
For such diseases that have a marked impact on both veterinary and medical fields (like psittacosis, cysticercosis etc), the approach that was taken in the reading for the week in New South Wales (Adamson, 2011) works really well. There can be effective collaboration between vets and physicians for prevention and preparedness, detection , analysis and response. However, it should not escape our notice that malaria is not listed as a notifiable disease by both the human and animal sectors, because many still strictly consider it an obligate human-mosquito pathogen.
With malaria caused by Plasmodium knowlesi however the NSW setup would work perfectly with physicians and wildlife experts filling in their expertise. This framework can be effective in P.knowlesi endemic areas , not so much in others because of differences in the niche occupied by the other Plasmodia.
Stakeholders in the One Health theory
Physicians, who are at the top of the 'health care access pyramid', should work together with researchers, epidemiologists and other stake holders (governmental and nongovernmental) . One example of a non governmental stake holder is the Bill and Melinda Gates Foundation, who support R&D financially by funding research grants (2 billion USD so far) for drug development, diagnostics, vector control methods and vaccines. They are partners with organizations such as the Global fund to Fight AIDS, tuberculosis and Malaria, Roll back Malaria, PATH Malaria Vaccine Initiative, Medicines for Malaria Venture, Malaria No more and Nothing but Nets. Such broad partnerships lay a broad resource network that can well be used to eradicate malaria soon. Although these private investors work on their own time frame and donate money for research, at the present time, there are no laws/ policies according to which they are expected to act.
This must be rectified and policy frameworks established to moderate everyone's role, without infringing on anyone's freedom to help, because financial gifts cannot be demanded.
The following pyramid from the Maternal and Child Health Program of the US Dept of Health and Human Services shows the essential features that must be covered by One Health policies for the eradication and management of disease. They can be adopted for malaria.
References :
1. Adamson S, Marich A, Roth I. One Health in NSW: coordination of human and animal health sector management of zoonoses of public health significance. N S W Public Health Bull 2011;22:105-112.
2. Ijumba JN, Lindsay SW. Impact of irrigation on malaria in Africa: paddies paradox. Med Vet Entomol 2001;15:1-11.
3. "Bill & Melinda Gates Foundation." Malaria. Gates Foundation, Seattle, 2013. Web. 18 Nov. 2013.
4. "MCH Programs Overview." MCH Programs Overview. Washington, 2013. Web. 19 Nov. 2013.
5. "The Manhattan Principles." cdc.gov. CDC, Atlanta, 2004. Web. 19 Nov. 2013.
6. "Contributing to One World, One Health.*" Undg.org. United Nation Development Group, 2008. Web. 19 Nov. 2013.
Tuesday, November 12, 2013
One Health - Sociology
The sociology of the one heath concept for malaria is built around human social behavior in the context of the disease's zoonotic nature. Of the five species of Plasmodium that can infect man (P.malariae, P.ovale, P.falciparum, P.vivax and P. knowlesi), P.knowlesi is a natural pathogen of long tailed and pig tailed macaques in South East Asia and hence considered a zoonosis. (CDC, 2013). There are numerous reports of the other Plasmodium species arising in the great apes and engulfing an ecological niche created by the movement of humans.
(Singh, 2013)
Although wild macaques are the original hosts of P.knowlesi, increased human depredations in forest areas has led to human infections. Some scientists theorize that in such an ecological mosaic such as the one that exists in SouthEast Asia, an increase in human interference could force a pathogenic species such as P.knowlesi to switch to humans as its preferred host. (Lee et al.,2011)
Since P.knowlesi multiplies every 24 hrs, cases of infection progress rapidly, often being fatal. The parasite resembles P.malariae (more benign) and is misdiagnosed as such, when diagnosis is based on microscopy. (Cox-Singh et al., 2008) Visitors entering endemic zones are at the highest risks.
Spread of the disease is influenced by many cultural factors as well. Due to population booms, much more of the forest land has been cleared for agricultural use, driving people and their animals to the edges of forests. People living in such close proximity to the jungle tend to enter it to forage for food, to gather firewood etc, where they encounter the infected mosquitoes.
There are two transmission cycles that ought to be addressed : (1) between macaques and (2) between humans and macaques. The latter occurs in the ecological mosaic where a vector that can bite both primates exists, which can transmit the parasite (Singh,2013; Thrusfield, 2007). Studies of this sort have involved entomologists, landscape epidemiologists, veterinarians etc. The conclusion that was reached was that the disease is transmitted to humans by mosquitoes that normally feed on animals and that human to human transmission does not seem to occur with the same vectors. It is exceedingly interesting to note that no urban outbreaks of P.knowlesi has occurred.
Management of such a zoonotic pathogen requires coordinated, consistent action from health professionals, scientists and the government, which is the basis of One Health. Further epidemiological studies are warranted. These must look at infection rates, describe intrinsic and extrinsic determinants, notify nosogenic territories, predict persistence and patterns of the disease. Surveillance must be undertaken by governmental agencies and health organizations. Trips into deep jungles by tourists, naturalists intent on discovering new species, military personnel undergoing jungle training and others must be kept to a minimum.
References :
4. Thrusfield, M. V. "7 : The Ecology of Disease." Veterinary Epidemiology. 3rd ed. N.p.: Blackwell, 2007. 116-36. Print.
5. Day MJ. One health: the importance of companion animal vector-borne diseases. Parasit Vectors 2011;4:49.
6. http://www.cdc.gov/malaria/about/biology/parasites.html
(Singh, 2013)
Although wild macaques are the original hosts of P.knowlesi, increased human depredations in forest areas has led to human infections. Some scientists theorize that in such an ecological mosaic such as the one that exists in SouthEast Asia, an increase in human interference could force a pathogenic species such as P.knowlesi to switch to humans as its preferred host. (Lee et al.,2011)
Since P.knowlesi multiplies every 24 hrs, cases of infection progress rapidly, often being fatal. The parasite resembles P.malariae (more benign) and is misdiagnosed as such, when diagnosis is based on microscopy. (Cox-Singh et al., 2008) Visitors entering endemic zones are at the highest risks.
Spread of the disease is influenced by many cultural factors as well. Due to population booms, much more of the forest land has been cleared for agricultural use, driving people and their animals to the edges of forests. People living in such close proximity to the jungle tend to enter it to forage for food, to gather firewood etc, where they encounter the infected mosquitoes.
There are two transmission cycles that ought to be addressed : (1) between macaques and (2) between humans and macaques. The latter occurs in the ecological mosaic where a vector that can bite both primates exists, which can transmit the parasite (Singh,2013; Thrusfield, 2007). Studies of this sort have involved entomologists, landscape epidemiologists, veterinarians etc. The conclusion that was reached was that the disease is transmitted to humans by mosquitoes that normally feed on animals and that human to human transmission does not seem to occur with the same vectors. It is exceedingly interesting to note that no urban outbreaks of P.knowlesi has occurred.
Management of such a zoonotic pathogen requires coordinated, consistent action from health professionals, scientists and the government, which is the basis of One Health. Further epidemiological studies are warranted. These must look at infection rates, describe intrinsic and extrinsic determinants, notify nosogenic territories, predict persistence and patterns of the disease. Surveillance must be undertaken by governmental agencies and health organizations. Trips into deep jungles by tourists, naturalists intent on discovering new species, military personnel undergoing jungle training and others must be kept to a minimum.
References :
1. Cox-Singh J, Davis TM, Lee KS, et al. Plasmodium knowlesi malaria in humans is widely distributed and potentially life threatening. Clin Infect Dis2008;46:165-171.
2. Lee KS, Divis PC, Zakaria SK, et al. Plasmodium knowlesi: reservoir hosts and tracking the emergence in humans and macaques. PLoS Pathog2011;7:e1002015.
3. Singh B, Daneshvar C. Human infections and detection of Plasmodium knowlesi. Clin Microbiol Rev 2013;26:165-184.
5. Day MJ. One health: the importance of companion animal vector-borne diseases. Parasit Vectors 2011;4:49.
6. http://www.cdc.gov/malaria/about/biology/parasites.html
Tuesday, October 22, 2013
Policy for anti-malarial chemotherapy
I was under the impression that the WHO and other international health organizations laid down (non-mandatory) policy guidelines for the treatment of malaria and that endemic countries did not really care about those guidelines. After all, doctors prescribe the medication and are trained to tailor it to the needs of their patient, right ? As I read on the subject though, I quickly found that the Medical Association and Health Department of every malaria-endemic country has it's own mandatory policy based on the WHO's guidelines.
An overview of the chemotherapy policies for different regions are listed on the WHO's website here. (WHO, 2013)
Even as early as 1990, the WHO had some "General considerations for the development of a malaria treatment policy". I have briefly discussed some of them here, but the considerations are not restricted to the ones listed below.
The seasonality of the disease and the level of acquired immunity in the population are epidemiological factors that must be accounted for in Rx policies. Severity of illness is severely influenced by the species of Plasmodium that has infected the person. Drug resistance too depends on the species, with P.falciparum being the most prone to develop drug resistance. So, prevalance and drug sensitivity studies are essential before polices are drafted.
Availability of malaria services in a region heavily influences the success of chemotherapeutic intervention policies. Malaria services are best implemented in association with general health services, than as stand alone programs. Such an integration, if necessary, must be spelled out clearly.
It is also essential to identify and define high risk groups/individuals, who would need prophylaxis. This would help in triage in outbreak settings and also in delivering radical curative treatment in unstable malaria areas.
Treatment regimens are also usually available in the policies , for different age groups and physiological conditions (pregnancy etc). However, these must be tailored to suit each individual patient's needs as many of the regimens are based on clinical trials and are not validated for field conditions. Regimens must take into account the medical supervision available for the treatment, that is, different forms of the drugs can/must be used for outpatients and some other forms are better suited for in-hospital administration.
Sociological aspects such as self medication must be taken into account too.
Unit cost of the drug and number of doses needed form the basis of the economy of chemotherapy Subsidies play a huge role in adherence to therapy regimens, by giving a pseudo-increase in buying power. But, even with subsidies and free medication, adherence is not 100%, which on a side note is one of the driving forces for resistance development.
Here is an example , from India, of the national drug policy against malaria :
The chemotherapy recommendations are given by the National Vector Borne Disease Control Programme, operating under the Ministry of Health & Family Welfare, Govt of India. The policy statement, in the 2013 edition, declares that one of the aims is "to minimize the risk of spread of drug resistant parasites by use of effective drugs in appropriate doses for everyone". With that goal in mind, the drug policy is intended to be "Appropriate for today and safe for tomorrow".
The ultimate goals of these policies are to provide complete clinical and parasitological cure of all malaria cases, prevent the progression of uncomplicated malaria into severe malaria and thereby reduce mortality, prevent relapse by administration of chemotherapeutic agents, interrupt transmission by the use of gametocytocidal drugs and prevent the development of drug resistant malaria .
References:
Neave PE, Taylor S, Behrens RH. Does public subsidy of the cost of malaria chemoprophylaxis reduce imported malaria? A comparative policy analysis. Malar J 2013;12:238.
Country antimalarial drug policies: by region. (n.d.). WHO. Retrieved October 22, 2013, from http://www.who.int/malaria/am_drug_policies_by_region_afro/en/index.html
National Vector Borne Disease Control Programme (NVBDCP). (n.d.). National Vector Borne Disease Control Programme (NVBDCP). Retrieved October 22, 2013, from http://nvbdcp.gov.in/
An overview of the chemotherapy policies for different regions are listed on the WHO's website here. (WHO, 2013)
Even as early as 1990, the WHO had some "General considerations for the development of a malaria treatment policy". I have briefly discussed some of them here, but the considerations are not restricted to the ones listed below.
The seasonality of the disease and the level of acquired immunity in the population are epidemiological factors that must be accounted for in Rx policies. Severity of illness is severely influenced by the species of Plasmodium that has infected the person. Drug resistance too depends on the species, with P.falciparum being the most prone to develop drug resistance. So, prevalance and drug sensitivity studies are essential before polices are drafted.
Availability of malaria services in a region heavily influences the success of chemotherapeutic intervention policies. Malaria services are best implemented in association with general health services, than as stand alone programs. Such an integration, if necessary, must be spelled out clearly.
It is also essential to identify and define high risk groups/individuals, who would need prophylaxis. This would help in triage in outbreak settings and also in delivering radical curative treatment in unstable malaria areas.
Treatment regimens are also usually available in the policies , for different age groups and physiological conditions (pregnancy etc). However, these must be tailored to suit each individual patient's needs as many of the regimens are based on clinical trials and are not validated for field conditions. Regimens must take into account the medical supervision available for the treatment, that is, different forms of the drugs can/must be used for outpatients and some other forms are better suited for in-hospital administration.
Sociological aspects such as self medication must be taken into account too.
Unit cost of the drug and number of doses needed form the basis of the economy of chemotherapy Subsidies play a huge role in adherence to therapy regimens, by giving a pseudo-increase in buying power. But, even with subsidies and free medication, adherence is not 100%, which on a side note is one of the driving forces for resistance development.
Here is an example , from India, of the national drug policy against malaria :
The chemotherapy recommendations are given by the National Vector Borne Disease Control Programme, operating under the Ministry of Health & Family Welfare, Govt of India. The policy statement, in the 2013 edition, declares that one of the aims is "to minimize the risk of spread of drug resistant parasites by use of effective drugs in appropriate doses for everyone". With that goal in mind, the drug policy is intended to be "Appropriate for today and safe for tomorrow".
The ultimate goals of these policies are to provide complete clinical and parasitological cure of all malaria cases, prevent the progression of uncomplicated malaria into severe malaria and thereby reduce mortality, prevent relapse by administration of chemotherapeutic agents, interrupt transmission by the use of gametocytocidal drugs and prevent the development of drug resistant malaria .
References:
Neave PE, Taylor S, Behrens RH. Does public subsidy of the cost of malaria chemoprophylaxis reduce imported malaria? A comparative policy analysis. Malar J 2013;12:238.
Country antimalarial drug policies: by region. (n.d.). WHO. Retrieved October 22, 2013, from http://www.who.int/malaria/am_drug_policies_by_region_afro/en/index.html
National Vector Borne Disease Control Programme (NVBDCP). (n.d.). National Vector Borne Disease Control Programme (NVBDCP). Retrieved October 22, 2013, from http://nvbdcp.gov.in/
Tuesday, October 15, 2013
Antimalarial drug resistance - Who is to blame?
Malaria treatment failure can arise either due to true antimalarial drug resistance or due to failure to clear malarial parasites from the circulation. The latter is due to incorrect dosing, non-compliance with the duration of dosing, poor drug quality , drug interactions, poor or erratic absorption and misdiagnosis. (Sosa, 2010)
The problem of misdiagnosis is essentially one of overdiagnosis. In many endemic countries, many febrile cases are prescribed antimalarial medication. A prospective observational study conducted in Afghanistan noted that 99% of the bloodsmear-negative patients received antimalarial medication when the diagnosis was based solely on clinical diagnosis. But even when blood smears were used for diagnosis, 50% of smear-negative patients received the medication. (Leslie, 2012). Many patients were thus unnecessarily exposed to the drugs and if they had had low parasitemia, there would have been enough selection pressure to cause drug resistance development.
Unregulated dispensing of drugs is another common problem and is frequently associated with the self-medication. In many developing countries, prescription medication can commonly be purchased over the counter. These include antibiotics and antimalarial drugs. Although there are laws to prevent such practices, these are almost always ignored. The ethics of pharmaceutical personnel are also questionable in these cases and may arise out of sheer ignorance of both pharmaceutical ethics and sound science.
Poverty driven practices are explored in the paper by Planta, M. , titled "The role of poverty in Antimicrobial resistance" , published in the Journal of American Board of Family Medicine, in Nov 2007. The author compares the practices in developing and developed nations. Noncompliance takes different forms in these cohorts, with the factors in developing countries being inadequate access to effective drugs, unregulated manufacture and dispensation of antimicrobials and lack of money to pay for appropriate, high quality medication. In contrast, the practices in developed countries mainly are sharing of antimicrobials and self medication using leftovers from unfinished drug regimens . (Planta MB, 2007). This was also explored at length in the reading for the day (McNulty,2007). Although both the articles explored antibacterial resistance, the same principles apply to sociology of antimalarial resistance.
Other factors that affect drug compliance include age, sex, martial status,educational level, ability to read and household monthly income. A demographical study of arteminisin combination therapy compliance conducted in rural Kenya revealed that only upto 47% of all malaria patients adhered to therapy, in terms of duration and dosage. Of these, 58% were <13 years of age. Adherence was higher among females (55.7%) than males (50.3%). Underaged patients (children) were the most adherent (57.1%), when compared to the married (21.4%), widowed (7.9%), single (2.9%), and separated (0.7%). (Onyango EO,2012) . This was probably because of higher concern among parents when the children are affected. Busyness and forgetfulness may be contributing factors among the older age groups, because no one intentionally wants to die of malaria, when they have access to medicines.Curiously, adherence increased as household size increased , with households with >6 people being more compliant than others. Undoubtedly, the statistics from this study cannot be extrapolated to wide regions across the globe. But, it gives a glimpse of the various factors that ought to be addressed when policies are laid down to overcome antimalarial resistance.
Increasing the awareness of people everywhere to antimicrobial resistance is an essential next step. Targeted education, information and communication activities are the need of the hour to reduce the risk of contributing to antimalarial resistance. Extension strategies used for doctors and health care workers, pharmaceutical personnel, policy makers and ordinary people residing in endemic areas must be specially designed to adequately cater to each group. Together, we can achieve our goal of overcoming antimalarial resistance.
References :
Leslie T, Mikhail A, Mayan I, et al. Overdiagnosis and mistreatment of malaria among febrile patients at primary healthcare level in Afghanistan: observational study. BMJ 2012;345:e4389.
Sosa AbdJ. Antimicrobial resistance in developing countries. New York: Springer, 2010.
Planta MB. The role of poverty in antimicrobial resistance. J Am Board Fam Med 2007;20:533-539.
McNulty CA, Boyle P, Nichols T, et al. The public's attitudes to and compliance with antibiotics. J Antimicrob Chemother 2007;60 Suppl 1:i63-68
Onyango EO, Ayodo G, Watsierah CA, et al. Factors associated with non-adherence to Artemisinin-based combination therapy (ACT) to malaria in a rural population from holoendemic region of western Kenya.BMC Infect Dis 2012;12:143.
Cartoons :
Dernavich, D. http://www.condenaststore.com/-sp/Woman-looking-at-pharmacy-shelves-labelled-Classics-Best-Sellers-and-New-Yorker-Cartoon-Prints_i8479870_.htm
Glasbergen, R. http://www.glasbergen.com/pharmacy-cartoons/
The problem of misdiagnosis is essentially one of overdiagnosis. In many endemic countries, many febrile cases are prescribed antimalarial medication. A prospective observational study conducted in Afghanistan noted that 99% of the bloodsmear-negative patients received antimalarial medication when the diagnosis was based solely on clinical diagnosis. But even when blood smears were used for diagnosis, 50% of smear-negative patients received the medication. (Leslie, 2012). Many patients were thus unnecessarily exposed to the drugs and if they had had low parasitemia, there would have been enough selection pressure to cause drug resistance development.
Unregulated dispensing of drugs is another common problem and is frequently associated with the self-medication. In many developing countries, prescription medication can commonly be purchased over the counter. These include antibiotics and antimalarial drugs. Although there are laws to prevent such practices, these are almost always ignored. The ethics of pharmaceutical personnel are also questionable in these cases and may arise out of sheer ignorance of both pharmaceutical ethics and sound science.
Poverty driven practices are explored in the paper by Planta, M. , titled "The role of poverty in Antimicrobial resistance" , published in the Journal of American Board of Family Medicine, in Nov 2007. The author compares the practices in developing and developed nations. Noncompliance takes different forms in these cohorts, with the factors in developing countries being inadequate access to effective drugs, unregulated manufacture and dispensation of antimicrobials and lack of money to pay for appropriate, high quality medication. In contrast, the practices in developed countries mainly are sharing of antimicrobials and self medication using leftovers from unfinished drug regimens . (Planta MB, 2007). This was also explored at length in the reading for the day (McNulty,2007). Although both the articles explored antibacterial resistance, the same principles apply to sociology of antimalarial resistance.
Other factors that affect drug compliance include age, sex, martial status,educational level, ability to read and household monthly income. A demographical study of arteminisin combination therapy compliance conducted in rural Kenya revealed that only upto 47% of all malaria patients adhered to therapy, in terms of duration and dosage. Of these, 58% were <13 years of age. Adherence was higher among females (55.7%) than males (50.3%). Underaged patients (children) were the most adherent (57.1%), when compared to the married (21.4%), widowed (7.9%), single (2.9%), and separated (0.7%). (Onyango EO,2012) . This was probably because of higher concern among parents when the children are affected. Busyness and forgetfulness may be contributing factors among the older age groups, because no one intentionally wants to die of malaria, when they have access to medicines.Curiously, adherence increased as household size increased , with households with >6 people being more compliant than others. Undoubtedly, the statistics from this study cannot be extrapolated to wide regions across the globe. But, it gives a glimpse of the various factors that ought to be addressed when policies are laid down to overcome antimalarial resistance.
Increasing the awareness of people everywhere to antimicrobial resistance is an essential next step. Targeted education, information and communication activities are the need of the hour to reduce the risk of contributing to antimalarial resistance. Extension strategies used for doctors and health care workers, pharmaceutical personnel, policy makers and ordinary people residing in endemic areas must be specially designed to adequately cater to each group. Together, we can achieve our goal of overcoming antimalarial resistance.
References :
Leslie T, Mikhail A, Mayan I, et al. Overdiagnosis and mistreatment of malaria among febrile patients at primary healthcare level in Afghanistan: observational study. BMJ 2012;345:e4389.
Sosa AbdJ. Antimicrobial resistance in developing countries. New York: Springer, 2010.
Planta MB. The role of poverty in antimicrobial resistance. J Am Board Fam Med 2007;20:533-539.
McNulty CA, Boyle P, Nichols T, et al. The public's attitudes to and compliance with antibiotics. J Antimicrob Chemother 2007;60 Suppl 1:i63-68
Onyango EO, Ayodo G, Watsierah CA, et al. Factors associated with non-adherence to Artemisinin-based combination therapy (ACT) to malaria in a rural population from holoendemic region of western Kenya.BMC Infect Dis 2012;12:143.
Cartoons :
Dernavich, D. http://www.condenaststore.com/-sp/Woman-looking-at-pharmacy-shelves-labelled-Classics-Best-Sellers-and-New-Yorker-Cartoon-Prints_i8479870_.htm
Glasbergen, R. http://www.glasbergen.com/pharmacy-cartoons/
Tuesday, October 8, 2013
The pharmacological basis of anti-malarial therapeutics
As we move into module 2 , "Chemotherapy and Resistance", we shift our focus from prophylaxis (prevention) to therapeutics (treatment). Chemotherapy, which is the use of chemical substances for therapy, against malaria is primarily available in the form of antiprotozoal drugs and anti-vector drugs (insecticides). This post will primarily focus on the drugs available and on resistance mechanisms.
There are three major classes of drugs that are clinically useful. Class I agents are used to treat or prevent clinically symptomatic malaria, but are not reliable against primary or latent liver stages or P.falciparum gametocytes.
Class II agents can target the asexual erythrocytic and the primary liver stages.
Class III agent can kill primary and latent liver stages as well as gametocytes.
The drugs are summarized below :
The timeline of drugs used against malaria, their introduction and establishment of resistance have been summarized (click to enlarge):
Current status :
Congeners of Chloroquine have been developed , which seem to be effective against chloroquine-resistant Plasmodium species. The antifolate drug combination (sulfadoxine and pyrimethamine) are still used in preventative therapy. Atovaquone and proguanil have recently also been used for prevention. Artemisinin and its derivatives form the core therapy primarily because of their speed of action, their efficacy against chloroquine-resistant Plasmodium and the additional effect of reducing transmission.
Drugs efficacious against P.falciparum is assumed to be effective against all the other Plasmodium species. However, the hypnozoite form of P.vivax can only be killed by treatment with primaquine.
Many other drugs and combinations are in clinical development. Example : NITD609, which is a spiroindolone that attacks the Na-ATPase PfATP4 is in Phase II trial.
Resistance mechanisms of Plamodium sps :
These have been summarized :

Abbreviations: PfCRT: P. falciparum chloroquine resistance transporter; PfMDR1: P. falciparum multidrug resistance transporter 1; PfMRP: P. falciparum multidrug resistance protein; CQ: chloroquine; AQ: amodiaquine; MQ: mefloquine; LM: lumefantrine; ART: artemisinin (and derivatives); KO: knock-out; RBC: red blood cell; P: parasite; DV: digestive vacuole.
References :
There are three major classes of drugs that are clinically useful. Class I agents are used to treat or prevent clinically symptomatic malaria, but are not reliable against primary or latent liver stages or P.falciparum gametocytes.
Class II agents can target the asexual erythrocytic and the primary liver stages.
Class III agent can kill primary and latent liver stages as well as gametocytes.
The drugs are summarized below :
The timeline of drugs used against malaria, their introduction and establishment of resistance have been summarized (click to enlarge):
Current status :
Congeners of Chloroquine have been developed , which seem to be effective against chloroquine-resistant Plasmodium species. The antifolate drug combination (sulfadoxine and pyrimethamine) are still used in preventative therapy. Atovaquone and proguanil have recently also been used for prevention. Artemisinin and its derivatives form the core therapy primarily because of their speed of action, their efficacy against chloroquine-resistant Plasmodium and the additional effect of reducing transmission.
Drugs efficacious against P.falciparum is assumed to be effective against all the other Plasmodium species. However, the hypnozoite form of P.vivax can only be killed by treatment with primaquine.
Many other drugs and combinations are in clinical development. Example : NITD609, which is a spiroindolone that attacks the Na-ATPase PfATP4 is in Phase II trial.
Resistance mechanisms of Plamodium sps :
These have been summarized :

References :
Ines Petersen, Richard Eastman, Michael Lanzer, Drug-resistant malaria: Molecular mechanisms and implications for public health, FEBS Letters, Volume 585, Issue 11, 6 June 2011, Pages 1551-1562
Tuesday, September 24, 2013
Policies for malaria vaccine
Policies in health management are very important for the day to day operation of any health organization. When dealing with diseases that are targeted for eradication by vaccination, like malaria, policies give a general direction in which to proceed. They include statements that identify the rules that govern vaccine manufacture and administration, and give reasons for why such rules exist. The policies are also expected to tell us when the vaccine rules apply and when they don't. They must tell us who is covered, who is not and the consequences of not being vaccinated.
Since an effective first generation vaccine against malaria is already in the works, (RTS,S/AS01 is in Phase III clinical trials right now), to begin utilizing it soon after licensure, severely affected endemic countries must have a time targeted policy in place by now.
The Malaria Vaccine Initiative (www.malariavaccine.org) has developed a tool for use by countries that helps expedite the decision making process. The tool, called the 'Malaria Vaccine Decision - Making Framework', helps in data collection, in time with the licensure process of the vaccine to ensure that the countries that need it are prepared and ready for it.
The tool basically divides data that can be collected into global data and national level data. Some of these like the impact of current interventions and their cost effectiveness are critical global data, that play a major part in the feasibility and success of eradication strategies. Other data such as national affordability, epidemiology profile by state/region/county are critical local data. By combining these, countries can start important processes and create the infrastructure needed. Important processes include establishing a technical working group at the national level, integrating the vaccine into the countries' multiyear strategic plan (on the basis of which funds get distributed at the national level), engaging local pharmaceutical companies, creating a national expert group on recommendations on vaccine introduction, creating advocacy groups, creating advertisements for extension activities etc.
References :
Malaria Vaccine Initiative http://www.malariavaccine.org/preparing-decision-making.php
http://www.malariavaccine.org/files/MVI-GSK-PhaseIIIfactsheetFINAL-web.pdf
Malaria Vaccine Decision making framework http://malvacdecision.net/2012/04/noor/
http://malvacdecision.net/see-the-progress-in-my-country/
http://malvacdecision.net/wp-content/themes/malaria-vaccine/DMF-data-and-processes-April2012.pdf
Since an effective first generation vaccine against malaria is already in the works, (RTS,S/AS01 is in Phase III clinical trials right now), to begin utilizing it soon after licensure, severely affected endemic countries must have a time targeted policy in place by now.
The Malaria Vaccine Initiative (www.malariavaccine.org) has developed a tool for use by countries that helps expedite the decision making process. The tool, called the 'Malaria Vaccine Decision - Making Framework', helps in data collection, in time with the licensure process of the vaccine to ensure that the countries that need it are prepared and ready for it.
The tool basically divides data that can be collected into global data and national level data. Some of these like the impact of current interventions and their cost effectiveness are critical global data, that play a major part in the feasibility and success of eradication strategies. Other data such as national affordability, epidemiology profile by state/region/county are critical local data. By combining these, countries can start important processes and create the infrastructure needed. Important processes include establishing a technical working group at the national level, integrating the vaccine into the countries' multiyear strategic plan (on the basis of which funds get distributed at the national level), engaging local pharmaceutical companies, creating a national expert group on recommendations on vaccine introduction, creating advocacy groups, creating advertisements for extension activities etc.
Deciding to set up a vaccine plan or policy takes considerable time. A country cannot decide suddenly that they want to begin using the vaccine, without any formal rules in place. The progress in policy making and setting up a framework has been different in different countries. Here are some updates from some African countries (I acknowledge that the sampling of countries is biased. I chose these countries because I have friends from these places):
Uganda : has a nation specific framework in place and has a committee on malaria vaccines, that was established in 2009, that meets regularly.
Ghana :Held kick off consultations, created a national framework for decision making, created a technical working group which has met regularly since 2009 and is working to collect data on malaria vaccine introduction. Ghana is also a Phase III clinical trial testing site.
Kenya : Has held national stakeholder consultations to discuss trials and have revised the framework to suit their national conditions and are in the process of creating a working group. Kenya is also a testing site for the phase III trials
Zimbabwe : is yet to set up plans
There are other endemic nations that are potential candidate countries for vaccine introduction, but are sitting on the fence right now, because of the unavailability of data from phase III trials and licensure proceedings. Also, other diseases may be on their priority list because of ease of elimination and the availability of a licensed vaccine. For example, malaria is endemic in India, but the government is not scrambling to get a policy in place to be able use the malaria vaccine upon licensure. Reasons include the facts that malaria is not high on the priority list, is curable, has a complex lifecycle that involves invertebrate vectors (which have to be eliminated) and has a lower disease burden in terms of hospital hours and lost work hours, than say chikungunya (which is also transmitted by mosquitoes). On the other hand, polio which has a cheap, effective oral vaccine, has proven itself as an eradicatable disease in other parts of the world and so is an easier target.(The Indian government has policies in place for polio vaccination, which is now mandatory, with no exemptions. The policies were drawn up as a part of a five year plan. The importance of incorporating vaccine policies into long term plans cannot be emphasised enough, because that is the only way something can be achieved).
In conclusion, vaccine policies are meant to build up the health of people and lift communities as a whole. Just as little drops make an ocean, small decisions made at the right time can cause effects that are greater than one's imagination.
References :
Malaria Vaccine Initiative http://www.malariavaccine.org/preparing-decision-making.php
http://www.malariavaccine.org/files/MVI-GSK-PhaseIIIfactsheetFINAL-web.pdf
Malaria Vaccine Decision making framework http://malvacdecision.net/2012/04/noor/
http://malvacdecision.net/see-the-progress-in-my-country/
http://malvacdecision.net/wp-content/themes/malaria-vaccine/DMF-data-and-processes-April2012.pdf
Monday, September 9, 2013
Vaccines - Sociological aspects
The readings for class 3 discussed some important reasons for the controversies that surround childhood vaccinations, highlighting issues such as vaccine ingredients, allergies and grouping these into nine pertinent categories. The readings also traced the roots of the problem and laid bare the theme at the center of it all : human nature.
With regard to the malarial vaccines, human social behaviour has been refined. Since there has been no vaccine commercially available so far, there has been no hue and cry yet.
The only malarial vaccine that has ever reached phase III clinical trials is the RTS,S, a subunit vaccine containing pre erythrocytic circumsporozoite protein (RTS) fused to the Hepatitis B surface antigen (B) (Lell B et al., 2009; WHO, 2009).
INTENDED TARGET GROUPS
The vaccine when commercially available will be primarily used in countries where malaria is endemic. In countries like the United States, where malaria is not endemic, the vaccine will probably be made available to people intent on travelling to international locations that are endemic.
WILL VACCINE EFFICACY PLAY A ROLE IN ITS ACCEPTABILITY ?
The vaccine at the heart of the childhood vaccine controversy , the MMR vaccine, has an efficacy of >90 percent. In phase II clinical trials conducted in Kenya and Tanzania, the RTS, S ,vaccine had an efficacy of only 52.9 % in children aged 5 to 17 months , who had been given a primary dose and two boosters. That is, only 53 people out of every 100 who are vaccinated could fight off an infection with wild type parasite. One could think that this could play a role in the acceptance of the vaccine by communities. It appears however that parents, in countries that are the intended target groups for the vaccine, perceive the risk of vaccination as being lower than the risk of contracting the disease itself.
Studies in central Ghana suggest that parents prefer the vaccine over prophylactic malarial drugs and that they are willing to add malarial vaccines to the myriad of other vaccines their children receive (Febir L et al., 2013).
AWARENESS GAPS .... WHERE EXPECTED, NONE EXIST !
Contrary to established narrow-minded expectations, field work in Mombazique showed that awareness about malaria and vaccines were very high. To quote Bingham et al., 2012, "Vaccines are seen as means to reduce the threat of childhood illnesses and to keep children and the rest of the community healthy"
Properly disseminated knowledge and the experience that stems from facing the deadly disease have made the target population wise. They do not seem to have fallen prey to their own intellect like the few in developed nations who reject childhood vaccinations.
THE THING WITH DOSES AND INGREDIENTS
So far, three doses of the vaccine are required to achieve effective immunity. If newer more efficacious adjuvants are not available soon, the cost of protection could be extraordinarily high. This can result in policy constraints in immunizing adults as well as children.
Also, since the vaccine has subunit antigens there will be no multiplication inside the vaccinated human and no spread of immunity (the spread of live vaccine poliovirus conferred immunity on exposed people as well). Herd immunity can be established only by vaccinating every individual.
To date, the adjuvant AS01, which contains monophosphoryl lipid A from LPS of Salmonella minnesota (Mata E. et al.,2013), has had a safe track record. But, if any adverse effect ever occurs, it can well be expected that the first ingredient in the vaccine that will be considered worthy of blame will be the adjuvant, since the proof of concept of using the RTS has been validated by use with other adjuvants such as AS02.
In conclusion, malarial vaccines will be well received when they are approved and marketed.
References
Lell B, Agnandji S, von Glasenapp I, Haertle S, Oyakhiromen S, Issifou S,
Vekemans J, Leach A, Lievens M, Dubois MC, Demoitie MA, Carter T, Villafana T,
Ballou WR, Cohen J, Kremsner PG. A randomized trial assessing the safety and
immunogenicity of AS01 and AS02 adjuvanted RTS,S malaria vaccine candidates in
children in Gabon. PLoS One. 2009 Oct 27;4(10):e7611.
Febir LG, Asante KP, Dzorgbo DB, Senah KA, Letsa TS, Owusu-Agyei S. Community
perceptions of a malaria vaccine in the Kintampo districts of Ghana. Malar J.
2013 May 7;12:156.
Bingham A, Gaspar F, Lancaster K, Conjera J, Collymore Y, Ba-Nguz A. Community
perceptions of malaria and vaccines in two districts of Mozambique. Malar J. 2012
Nov 28;11:394.
Mata E, Salvador A, Igartua M, Hernández RM, Pedraz JL. Malaria vaccine
adjuvants: latest update and challenges in preclinical and clinical research.
Biomed Res Int. 2013;2013:282913. doi: 10.1155/2013/282913. Epub 2013 Apr 23.
PubMed PMID: 23710439; PubMed Central PMCID: PMC3655447.
With regard to the malarial vaccines, human social behaviour has been refined. Since there has been no vaccine commercially available so far, there has been no hue and cry yet.
The only malarial vaccine that has ever reached phase III clinical trials is the RTS,S, a subunit vaccine containing pre erythrocytic circumsporozoite protein (RTS) fused to the Hepatitis B surface antigen (B) (Lell B et al., 2009; WHO, 2009).
INTENDED TARGET GROUPS
The vaccine when commercially available will be primarily used in countries where malaria is endemic. In countries like the United States, where malaria is not endemic, the vaccine will probably be made available to people intent on travelling to international locations that are endemic.
WILL VACCINE EFFICACY PLAY A ROLE IN ITS ACCEPTABILITY ?
The vaccine at the heart of the childhood vaccine controversy , the MMR vaccine, has an efficacy of >90 percent. In phase II clinical trials conducted in Kenya and Tanzania, the RTS, S ,vaccine had an efficacy of only 52.9 % in children aged 5 to 17 months , who had been given a primary dose and two boosters. That is, only 53 people out of every 100 who are vaccinated could fight off an infection with wild type parasite. One could think that this could play a role in the acceptance of the vaccine by communities. It appears however that parents, in countries that are the intended target groups for the vaccine, perceive the risk of vaccination as being lower than the risk of contracting the disease itself.
Studies in central Ghana suggest that parents prefer the vaccine over prophylactic malarial drugs and that they are willing to add malarial vaccines to the myriad of other vaccines their children receive (Febir L et al., 2013).
AWARENESS GAPS .... WHERE EXPECTED, NONE EXIST !
Contrary to established narrow-minded expectations, field work in Mombazique showed that awareness about malaria and vaccines were very high. To quote Bingham et al., 2012, "Vaccines are seen as means to reduce the threat of childhood illnesses and to keep children and the rest of the community healthy"
Properly disseminated knowledge and the experience that stems from facing the deadly disease have made the target population wise. They do not seem to have fallen prey to their own intellect like the few in developed nations who reject childhood vaccinations.
THE THING WITH DOSES AND INGREDIENTS
So far, three doses of the vaccine are required to achieve effective immunity. If newer more efficacious adjuvants are not available soon, the cost of protection could be extraordinarily high. This can result in policy constraints in immunizing adults as well as children.
Also, since the vaccine has subunit antigens there will be no multiplication inside the vaccinated human and no spread of immunity (the spread of live vaccine poliovirus conferred immunity on exposed people as well). Herd immunity can be established only by vaccinating every individual.
To date, the adjuvant AS01, which contains monophosphoryl lipid A from LPS of Salmonella minnesota (Mata E. et al.,2013), has had a safe track record. But, if any adverse effect ever occurs, it can well be expected that the first ingredient in the vaccine that will be considered worthy of blame will be the adjuvant, since the proof of concept of using the RTS has been validated by use with other adjuvants such as AS02.
In conclusion, malarial vaccines will be well received when they are approved and marketed.
References
Lell B, Agnandji S, von Glasenapp I, Haertle S, Oyakhiromen S, Issifou S,
Vekemans J, Leach A, Lievens M, Dubois MC, Demoitie MA, Carter T, Villafana T,
Ballou WR, Cohen J, Kremsner PG. A randomized trial assessing the safety and
immunogenicity of AS01 and AS02 adjuvanted RTS,S malaria vaccine candidates in
children in Gabon. PLoS One. 2009 Oct 27;4(10):e7611.
Febir LG, Asante KP, Dzorgbo DB, Senah KA, Letsa TS, Owusu-Agyei S. Community
perceptions of a malaria vaccine in the Kintampo districts of Ghana. Malar J.
2013 May 7;12:156.
Bingham A, Gaspar F, Lancaster K, Conjera J, Collymore Y, Ba-Nguz A. Community
perceptions of malaria and vaccines in two districts of Mozambique. Malar J. 2012
Nov 28;11:394.
Mata E, Salvador A, Igartua M, Hernández RM, Pedraz JL. Malaria vaccine
adjuvants: latest update and challenges in preclinical and clinical research.
Biomed Res Int. 2013;2013:282913. doi: 10.1155/2013/282913. Epub 2013 Apr 23.
PubMed PMID: 23710439; PubMed Central PMCID: PMC3655447.
Wednesday, September 4, 2013
An overview of vaccines against malaria
IN THE NEWS
On 9 August 2013, CNN reported a breakthrough in malaria
vaccinology. A new radiation attenuated intravenous vaccine has shown to be 100
% efficacious if injected in multiple doses. In about eight to ten years, this
vaccine would be readily available at any pharmacy store. Before that, it has
to pass rigorous tests of safety and must be approved by the FDA.
ARE WE THERE YET ?
Although it is relatively easy to produce updated flu
vaccines every year, malaria vaccines have eluded decades of research. There
have been many hurdles along the way. Some of these have been discussed in a
paper by Thera and Plowe, titled "Vaccines for Malaria: How close are we?
" published in the Annual Reviews in Medicine in November 2011.
The first obstacle is the size of the parasite's genome. The
5000 genes in Plasmodium falciparum's genome are organized into 14 chromosomes
and there are roughly 23 million bases. This precludes the development of an
efficient DNA vaccine. Successful DNA vaccines have so far only been developed against
viruses and bacteria with much smaller genomes.
The complex lifecycle of Plasmodium also allows for differential
gene expression. Like the Lyme disease parasite that shows antigenic (and phase
variation), Plasmodium expresses highly variant antigens such as PfEMP1s that
are coded by up to 60 var genes in the genome.
In the haploid liver stages and blood stages of the
parasite, mutations occur during mitotic replication. Genetic recombination
commonly occurs during the diploid sexual stages. Drugs used against Plasmodium
also provide some amount of selection pressure and drive mutation of the
parasite. From a single geographical location, it is possible to isolate up to
18 different forms of a surface antigen. Hence, potential surface epitope
change and when these vaccine targets are lost or modified, older vaccines (in
the case of malaria, which were never available to begin with) become obsolete.
Polymorphisms in surface antigens play important roles in
determining strain specific immunity.
Malaria vaccines typically target a specific stage of the
parasitic lifecycle and show effect only against that stage. However, even a
single surviving parasite such as a sporozoite could multiply to produce
thousands of merozoites in 48 hours and result in an infection.
THE STORY SO FAR ..
Vaccines against malaria that have
been experimentally created fall under these main categories. Classification is
based on the stage of protection, rather than the conventional classification of vaccine type.
> Pre Erythrocytic vaccines
>Blood stage vaccines
>Transmission blocking vaccines
PRE ERYTHROCYTC VACCINES
RTS,S/ AS01 is an experimental subunit vaccine that targets
the pre-erythrocytic circumsporozite protein CSP of Plasmodium falciparum. It
consists of CSP (which has a central conserved region flanked by T cell
epitopes) in Adjuvant System 01 (a proprietary adjuvant that contains
monophosphoryl lipid A and QS21). This vaccine showed up to 60 % protection in
field trials. It is currently in phase III trials in seven African countries.
To offer substantial protection, subunit vaccines have to be
combined with strong adjutants. This in itself poses a risk of severe reactions
against the adjuvant.
Other pre-erythrocytic vaccines that have passed preclinical
and early clinical trials have not shown too much promise.
BLOOD STAGE VACCINES
These are usually based on antigens that coat the surface of
the invasive merozoites or are involved in the hijacking of the erythrocyte.
The merozoite surface protein 1 or MSP1 and the apical membrane antigen 1 or
AMA 1 has both shown some promise as vaccine candidates.
Two AMA1 vaccines have passed the preclinical and clinical
stages of development.
A vaccine directed against merozoites surface protein 3 has shown
some efficacy against the clinical stage of malaria.
TRANSMISSION BLOCKING VACCINES
These vaccines target immunogenic epitopes on gametocytes
and other mosquito stages that are important for the transmission of the
parasite.
Although one such vaccine appeared to produce immunity by
blocking transmission, the adjuvant that it was formulated with viz., Contained
ISA 51 created safety issues by being extremely reactive.
MULTI STAGE MULTI ANTIGEN VACCINES
Plasmodium is a complex organism and so to be efficacious
against different stages, a vaccine must target different antigens that are
immunodominant at different stages of the organism.
SPf66 is one such vaccine. It is a synthetic vaccine that
targets the CSP expressed in the pre-erythrocytic stage. SPf66 is derived from
the MSP1 and hence is also protective in the erythrocytic stages.
WHOLE ORGANISM VACCINES
Although one would assume that this would be the direct
approach to a vaccine against malaria, some of the early trials in which whole
organisms were used were not interpreted as a direct path to a vaccine.
However, the report on CNN concerned a vaccine that was made
from radiation attenuated, metabolically active, non-replicating cryopreserved
sporozoites. This vaccine did not show protection when injected via the
intradermal or subcutaneous routes. Intravenous route that mimicked the bite of
a female mosquito showed the best effect. After delivery, the sporozoites were
able to reach and replicate in the liver and induce protection.
A list of antigenic candidates that can be targeted and used in a vaccine are listed here : http://www.hindawi.com/journals/bmri/2013/282913/tab2/
A list of antigenic candidates that can be targeted and used in a vaccine are listed here : http://www.hindawi.com/journals/bmri/2013/282913/tab2/
THE START OF A JOURNEY
Developing an efficient vaccine against malaria is not an
end by itself. The vaccine is only a tool that will be useful in combating the
deadly disease and will help in its eradication.
References :
Thera MA, Plowe CV. Vaccines for malaria: how close are we? Annu Rev Med 2012;63:345-357.
Malaria vaccine initiative : http://www.malariavaccine.org/malvac-lifecycle.php
References :
Thera MA, Plowe CV. Vaccines for malaria: how close are we? Annu Rev Med 2012;63:345-357.
Malaria vaccine initiative : http://www.malariavaccine.org/malvac-lifecycle.php
Malaria - the disease
Etiology
Malaria is caused by protozoae of the genus Plasmodium. It was
traditionally believed that there are only four species that cause human malaria:
Plasmodium falciparum, P. malariae, P.ovale and P.vivax. (WHO, 2013). A fifith
species was isolated in 2010 and has been named P. knowlesi. (Kantele
A, 2010). The four species have distinct morphological differences that aid in
their diagnosis on a blood smear. (CDC, 2013).
Malaria is vector borne and the parasites can be
transmitted by more than thirty species of Anopheline mosquitoes.
Epidemiology
Malaria is endemic in 104 countries . (WHO, 2012)
The average incubation period for malaria is 12
days (tropical strains) and 15 days (Temperate strains). (Lover AA,
2013)
Malaria
is severe in children , immunosuppressed patients and pregnant women. Malaria
in pregnant women can cause miscarriages, stillbirths and neonatal death. (WHO,
2013)
Lifecycle
Infectious sporozoites of the Plasmodium are
carried by the Anopheles mosquito in its salivary glands. When the mosquito
feeds on a human, it injects saliva and the sporozoites into the body. The
sporozoites moves to their predilection site , the liver. There the sporozoites
enter the hepatocytes and divide. They produce thousands of merozoites , which
are haploid forms. These rupture the hepatocytes as they exit and enter the
blood stream.
Erythrocyte invasion by merozites (Haldar et al.,2007)
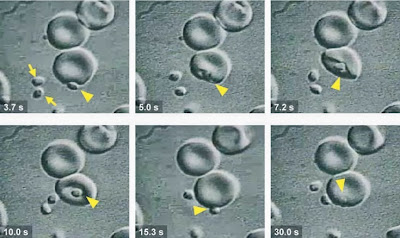
The intraerythrocytic cycle of Plasmodium is clinically important. The receptors on the erythrocytes include Thrombospondin, CD36, ICAM-1, VCAM-1 and ELAM-1.(Pasloske, 1994). The erythrocytes infected with mature stages of Plamodium adhere to vascular endothelial cells in postcapillary venules. Infected erythrocytes can also form rosettes with uninfected erythrocytes. In P.falciparum, the paraite matures to a trophozoite stage, which matures into schizonts, which eventually relaease 16-32 daughter merozoites on rupturing the RBC. These merozoites invade uninfected erythrocytes and the cycle continues.
Malaria : Clinical stages
The acute disease presents as a febrile sickness.
(WHO,2013). The intra erythrocytic cycle of the parasite is reflected as a
cyclic pattern of fevers and chills. Other features of the disease include
hypoglycemia, hyperlactermia, anemia and altered consciousness (Weatherall DJ, 2002 ; Haldar, 2006). Levels of TNF alpha are high in malaria patients.
TNF alpha enhances the expression of ICAM-1, VCAM-1 and ELAM-1 and is
responsible for causing prodromal symptoms such as fever and nausea (Pasloske, 1994)
The most severe disease is caused by P. falciparum.
Clinical signs are nonspecific and include fever, chills, headaches, myalgia,
vomoitng, cough , abdominal pain. Complications that arise from this infection
include acute renal failure, pulomnary oedema, convulsons, shock, coma and
death. Cerebral malaria is a complicated form of
Plasmodium falciparum infection, found especially in children.
Malaria
caused by P.vivax and P.ovale are not as life threatening as falciparum malaria but are the major cause for relapsing
malaria. These protozoae can remain dormant in the liver as persistent liver
forms called hypnozoites. (WHO,2013)
Diagnosis
The
WHO recommends definitive diagnosis either on the basis of microscopy or rapid
diagnostic tests.Plasmodium species can be detected on blood smears stained by simple Romanowsky stains such as Giemsa. Blood smears are easy and inexpensive to make. This method allows detection of various stages of the parasite and a rough quantification of parasite density. (WHO, 2013)
The Rapid Detection Tests detect specific antigens in the serum/blood. These tests can detect a single species at a time or multiple Plasmodium species.
Treatment
The disease is entirely preventatble and treatable. According to the " Guidelines for the Treatment of Malaria " Handbook published by the WHO in 2010, Arteminisin based combination therapies are recommended for uncomplicated cases. Combination therapies include Artemininsin in combination with lumefantrine, amodiaquine, mefloquine, sulfadoxine-pyrimethamine. Duration of therapy must be atleast seven days.
Second line treatments recommended are artesunate with tetracycline/ doxycycline / clindamycin for 7 days.
Prevention
The
main method of prevention so far has been vector control. Mosquitoes can be
eliminated by insecticide spraying on breeding grounds. Transmission can be
prevented by the use of individual insecticide treated mosquito nets.
Vaccines
Subunit vaccines against
malaria are being evaluated in clinical trials. These will be explored in subsequent posts.
malaria]. Duodecim. 2010;126(4):427-34.
Weatherall DJ, Miller LH, Baruch DI, Marsh K, Doumbo OK, et al. 2002.
Malaria and the red cell. Hematology
Am. Soc. Hematol. Educ. Program 1:35–57
Pasloske BL, Howard RJ. Malaria, the red cell and the endothelium. Annu Rev Med. 1994; 45: 283-95
Haldar K, Murphy SC, Milner DA, Taylor TE. Malaria : mechanisms of erythrocytic infection and pathological correlates of severe disease. Annu Rev Pathol. 2007; 2 : 217-49
Lover AA, Coker RJ. Quantifying effect of geographic location on
epidemiology of Plasmodium vivax malaria.
Emerg Infect Dis [Internet]. 2013 JulPasloske BL, Howard RJ. Malaria, the red cell and the endothelium. Annu Rev Med. 1994; 45: 283-95
Haldar K, Murphy SC, Milner DA, Taylor TE. Malaria : mechanisms of erythrocytic infection and pathological correlates of severe disease. Annu Rev Pathol. 2007; 2 : 217-49
WHO World Malaria Report 2012 (who.int/malaria/publications/world_malaria_report_2012/en/)
Subscribe to:
Posts (Atom)